
What is enthesitis?
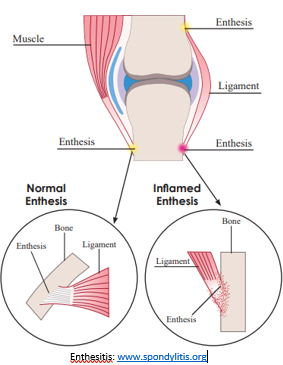
Enthesitis is an inflammation of the enthesis, the point where a connective tissue such as a ligament or tendon attaches to a bone. There are over 100 entheses in the body.
One in three people with psoriatic arthritis (PsA) will develop enthesitis. The presence of enthesitis is often used to help diagnose PsA.
What are the symptoms?
Enthesitis causes pain at the enthesis that gets worse with movement. Stiffness of the surrounding joints is also common. It can also cause bone spurs - an abnormal bone growth on the edge of a bone. This can add to the pain and discomfort.
Enthesitis can affect any enthesis in the body. For people with PsA, it commonly causes pain in the heel or the sole of the foot. This is because it can affect the point where the Achilles tendon attaches to the back of the heel or at the bottom arch of the foot along the plantar fascia (ligament that attaches the heel to the front of the foot).
What are the causes?
The same inflammatory process that causes your joints to become swollen and sore in PsA can also cause enthesitis.
Enthesitis can affect anyone, but it is more common in people with PsA. Repeated stress on an enthesis can cause damage to build up over time, which triggers the inflammation. For most people this would normally heal with ice and rest. For people with PsA this normal healing process may not happen. This can lead to the inflammation becoming chronic (continuing over a long period of time).
One in three people with PsA will develop enthesitis and it is more common in people with PsA than in people with other forms of arthritis.
How is it diagnosed?
For most people, their medical history and symptoms are enough to diagnose enthesitis. Simple tests may also be used such as checking if the pain worsens when moving or when pressure is put on the joint. Your doctor may also send you for some medical images, such as an ultrasound or x-ray to help confirm the condition.
What will happen to me?
Enthesitis can be an indicator of greater disease activity in people with PsA. This means that if you have enthesitis, you may also have more inflammation, pain and fatigue related to your PsA. It is important to work with your rheumatologist to find a treatment plan that works for you.
You may find enthesitis impacts your quality of life. Discuss these impacts with your doctor. They can refer you to another health professional, such as a podiatrist, occupational therapist or psychologist.
Can it be cured?
The level of pain and stiffness due to enthesitis can vary over time and may resolve naturally or with treatment. However, enthesitis caused by PsA is likely to reoccur or ‘flare’. The aim of treatment is to manage your arthritis, and the symptoms of enthesitis to minimise the impacts on your quality of life.
What treatments are there?
Your doctor may start treatment with nonsteroidal anti-inflammatory drugs (known also as NSAIDs). These may be tablets, or creams that are applied directly to the site of the enthesitis. NSAIDs can help to relieve the inflammation and pain. However, the long-term use of NSAIDs is not recommended as they can have unwanted side effects.
Your doctor may also give you a cortisone injection into the affected area.
Longer term treatment may involve taking a biologic disease modifying anti-rheumatic drug (biologic or bDMARD). The aim of these medications is to control the underlying PsA.
What can I do?
There are things you can do to reduce the pain and discomfort of enthesitis.
- Ensure that your PsA is well-managed. This will also help to keep the inflammatory process that causes enthesitis under control.
- Try to keep exercising. Exercise maintains our overall health and fitness and can help manage pain by releasing endorphins (chemicals naturally produced by the body to relieve stress and pain).
- It can be difficult to start or continue exercising when you are in pain. Speak with an exercise physiologist or physiotherapist to figure out an exercise plan that works for you.
- You may find that icing the affected areas can help.
- Try to maintain a healthy weight. Excess weight can put additional pressure on painful joints. The website, https://livelighter.com.au/ is a good source for healthy recipes.
- If it affects your feet, speak with a podiatrist. They can help you with how to best care for your feet, including the use of orthotics or specific footwear.
- Speak with an occupational therapist about how to manage fatigue.
- Speak with your doctor if you have any questions about your prescribed treatments or about your condition.
- Speak with your doctor about seeing a counsellor or psychologist if you need to talk to someone about the impact your condition is having on your mental wellbeing.
This article was developed based on the best available evidence. A full list of references is available on request.










