What is uveitis?
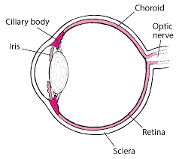
Uveitis is an inflammation of the middle layer of the eye, known as the uvea.
The uvea is made up of different parts, including the iris at the front, the choroid at the back, and the ciliary body in between.
Iritis is inflammation of the iris and is the most common form of uveitis.
What are the symptoms?
Symptoms of uveitis include:
- Redness
- Eye pain
- Sensitivity to light
- Watering of the eyes or teary eyes
- Black dots in the vision (can also be referred as floaters)
- Blurry vision
- A pupil that is smaller than normal.
Symptoms may occur in just one eye or in both eyes at the same time.
What causes uveitis?
Uveitis can be caused by eye infections or by other eye problems such as scratch to the cornea (front part of eye). For people with psoriatic arthritis (PsA) it is often caused by the same process that causes inflammation of the joints.
Uveitis is estimated to affect up to one in four people who have PsA. Smoking can also increase the chance of developing it.
How is it diagnosed?
Your doctor will diagnose uveitis by talking to you about your symptoms and asking about your other medical conditions. If you are already seeing an optometrist, they may also pick up changes in your eye. Your doctor will likely refer you to an ophthalmologist to have the condition confirmed by a thorough eye exam. An ophthalmologist is a medical doctor who specialises in the diagnosis and management of eye conditions. The ophthalmologist will work with you and your healthcare team to figure out the best treatment for you.
What will happen to me?
For most people uveitis can be managed with the right treatment. There will be times when the inflammation and symptoms are minimal. At other times, symptoms may worsen. This is more likely to happen when PsA symptoms also worsen or ‘flare’.
Some cases can cause long-term damage to the eye. While uncommon, permanent vision loss can occur. In most cases these long-term complications can be avoided, if uveitis is diagnosed and treated early. It is important to see your doctor should you experience symptoms.
Can uveitis be cured?
At times you may experience no signs or symptoms of uveitis, however it is not curable, except when caused by a bacterial infection. The aim of treatment is to control the symptoms and prevent long-term damage and complications.
What treatments are there for uveitis?
There are two main medications that are used to treat uveitis. Your ophthalmologist will prescribe either of the following, or a combination of the two:
- Corticosteroids to reduce eye inflammation.
- Eye drops or cream that dilate (enlarge) the pupil to prevent it sticking to the lens of the eye and causing scarring.
In addition, if you are not already taking them for your PsA, medications to reduce inflammation may be recommended to treat the underlying cause. Your rheumatologist will be able to discuss this with you.
What can I do?
Here are some things that you can do to reduce the risk of long-term complications:
- Ensure that your PsA is well-managed. This will also help keep the inflammatory process that causes uveitis under control.
- Take your medications as prescribed as this will reduce the risk of long-term damage to your eyes..
- Ask your ophthalmologist how often you need to see them.
- Speak with your doctor if you have any questions about your prescribed treatments or about the condition.
- When discussing possible treatments, you may want to ask your doctor:
- How long it will take for your medication to start working? With some medications it can take several weeks before your condition improves.
- What are some of the possible side effects? What the signs of these side effects are and what you should do if you are experiencing a side effect?
- When you can stop taking your medication? Some medication may need to be taken until the symptoms go away while others may need to be taken for longer.
- Tell your doctor about any medication you are taking, including complementary medications (such as vitamins, herbal medicines). Some medications taken together can cause unwanted side effects.
- Speak with your doctor about seeing a counsellor or psychologist if you feel you need to talk to someone about how your mental wellbeing is affected.
This resource has been developed based on the best available evidence. A full list of references is available upon request.










