
Most people with psoriatic arthritis (PsA) will also have psoriasis. Psoriasis causes itchy, red or silver scaly patches on the skin. Like PsA, psoriasis is an autoimmune condition. This means your immune system becomes overactive and attacks healthy tissues.
Although psoriasis cannot be cured, symptoms can reduce or disappear with treatment. A range of treatments is available. These include creams and ointments that you use on your skin, called topical treatments; phototherapy (light therapy); and medicines. Some medicines for PsA also work for psoriasis.
The best treatment for you depends on a number of factors. These factors include how severe your psoriasis is, where it is on you body, how it affects your quality of life, and whether you have other health concerns. Speak to your GP or dermatologist about your treatment options for psoriasis.
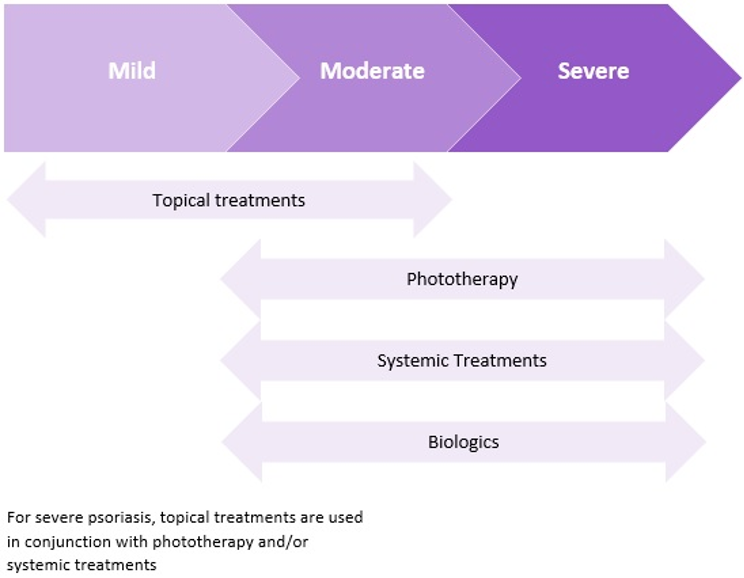
The diagram below shows the type of treatment usually recommended depending on the severity of psoriasis:
Topical therapies
Topical treatments are usually the first treatments prescribed for psoriasis. They help to reduce itching and control inflammation by slowing the growth of skin cells. They include gels, creams, lotions and ointments which come in different strengths. Lower-strength products can be bought over-the-counter at the chemist. You may need a prescription for higher-strength products. Your doctor may suggest you use one or more of these treatments.
Topical treatments are often used alongside other treatments.
Common topical treatments
- Corticosteroids (cortisone creams). These are the most common topical treatments for psoriasis. They reduce inflammation of the skin.
- Calcipotriol is a form of Vitamin D that encourages healthy skin growth.
- Coal tar is often used to treat scalp psoriasis. It slows the growth of skin cells and reduces inflammation, itchiness and dry skin. It comes in a range of shampoo products, oils and creams.
- Salicylic acid helps to loosen dry, scaly skin so it is easier to remove. This allows other treatments to be more easily absorbed.
In addition, moisturisers and emollients (skin softeners) can help to reduce itching by moisturising and softening the skin.
Phototherapy
Phototherapy (light therapy) uses ultraviolet (UV) rays, like those produced by the sun, to slow the growth of skin cells. It is generally used for moderate to severe psoriasis when topical treatments aren’t enough.
The treatment can only be provided by a dermatologist at their clinic. You may need to attend a few times a week for 6-10 weeks.
A few factors need to be considered to decide if phototherapy is suitable for you. These include the colour of your skin and how it reacts to sunlight, your other medical conditions and whether you are taking any medicines that make you more sensitive to light.
Medicines
If other treatments do not control your symptoms, you may be prescribed systemic treatments. These are medicines that work throughout the whole body.
There are two main categories: standard treatments, which are usually taken as tablets or capsules, and ‘biologic’ treatments, which are usually given as an injection.
Most of these medicines work by reducing the activity of the immune system to reduce inflammation (known as immunosuppression). Some may improve both psoriasis and psoriatic arthritis.
Standard systemic treatments
Standard systemic treatments include
- Acitretin: a type of medicine that is closely related to vitamin A and helps to slow down the growth of new skin cells.
- Medicines known as disease-modifying anti-rheumatic drugs (DMARDs), which reduce the activity of the immune system.
- Ciclosporin
- Methotrexate
- Apremilast
Methotrexate and apremilast also help to control joint pain and swelling in PsA.
Biologic treatments
Biologic treatments, also known as biologic DMARDs, are used for severe cases of psoriasis and PsA. They work by blocking the action of specific parts of the immune system. There are different biologic medicines that work on different parts of the immune system. Biologics are taken by injection.
Things you can do
One of the best things you can do to manage your psoriasis and/or psoriatic arthritis is stick to the treatment plan prescribed by your GP or specialist. There are also lifestyle changes you can make that may have a positive impact on your condition, as well as help you cope better.
Below, are some suggestions that you might find helpful:
- Manage your stress levels. Stress is a trigger for symptom flare-ups, so do what you can to reduce and manage your stress levels. Watch our video relaxation strategies for more information.
- Try to prevent skin ‘damage’. Cuts, insect bites, scratching and even sunburn can all trigger a psoriasis flare.
- Track your triggers. Keeping a health journal can help you figure out what triggers a psoriasis flare.
- Quit smoking. Smoking increases the risk of developing both psoriasis and PsA and can make both conditions worse. For advice and help to quit smoking, call the Quitline on 13 78 48 or visit quitnow.gov.au. Read How smoking could be worsening your symptoms for more information.
- Avoid drinking too much alcohol. Drinking too much alcohol can also make psoriasis worse. For adults, experts recommend no more than two standard drinks per day.
- Stay active and eat well. Exercise improves mood and sleep quality and helps to reduce stress. Eating a health balanced diet can help maintain good general health. Read our resources on Things you can do for information on maintaining a healthy lifestyle.
- Aim for and maintain a healthy body weight. Treatments for psoriasis are less effective if people are overweight. Exercise, diet and weight reduction can increase treatment effectiveness. Read Importance of maintaining a healthy weight for more information.
- Take care of your overall health. People with psoriasis and psoriatic arthritis are at higher risk of developing other chronic and serious health conditions, also known as co-morbidities.
This resource was developed based on the best available evidence. A full list of references is available on request.










